
The aorta is the largest artery in the body, carrying blood from the heart to the rest of the body. An Aortic Aneurysm (AA) develops when the wall of the aorta weakens and begins to bulge outwards. Aneurysms can occur in different regions, including the chest, as a Thoracic Aortic Aneurysm (TAA), the abdomen, as an Abdominal Aortic Aneurysm (AAA), or between the chest and abdomen, as a Thoracoabdominal Aortic Aneurysm (TAAA). While small aneurysms may not be immediately dangerous, larger ones can rupture, causing severe internal bleeding and potentially death.
- Persistent pain in the chest, abdomen, back, or lower limbs
- Fever
- Pulsating or throbbing mass in the abdomen
- Gangrene patches in the toes
- Recurrent vomiting after eating
- Chronic smoking
- Age over 65 (predominantly males)
- Long-term hypertension or heart disease
- Soft tissue diseases such as Marfan syndrome, Ehlers-Danlos syndrome, Loeyz-Dietz syndrome
- Family history of aortic aneurysms
Diagnosis involves clinical examination followed by imaging tests like ultrasound or CT scans.
Treatment options:
The traditional treatment method is open surgical repair. This is the conventional method of aneurysm repair, but has significant morbidity and mortality risks due to its invasive nature. Hence, it is recommended only for younger patients with low surgical risk. Post-surgery recovery usually requires ICU care for up to 1 week. Patients generally take about one month to 6 weeks for full recovery.
VIC offers a minimally invasive procedure known as Endo-Vascular Aortic Repair (EVAR). It involves the insertion of special stents (small tubes that hold the vessel open) through the leg femoral arteries via small incisions in the groin into the site of the aneurysm, relining the stent and excluding it from the arterial blood pressure circulation under X-ray guidance (fluoroscopy). EVAR can be done for older patients or patients who have higher surgical risks due to its minimally invasive nature, and can be done under local anaesthetic and mild sedation. Patients who undergo EVAR usually do not require ICU stay and are usually up and about in 8 hours. They usually can be discharged 48 hours post-surgery.
Follow up care:
Regular follow-ups are recommended for patients for the rest of their life after treatment of the AA, as the disease can continue to develop in other parts of the aorta that were previously aneurysm-free. It is possible for a patient with an abdominal aneurysm to then develop a thoracic aneurysm and vice versa. This risk is exacerbated if the patient still has persistent risk factors such as smoking and hypertension. Follow-up post aneurysm procedures include scanning for any further discrepancies at regular intervals (to be done 6 monthly at first, then annually). This is especially important for patients who have undergone the EVAR procedure.
Case Study 1
Patient presented with a pulsatile central abdominal mass. CT Scan showed an infrarenal abdominal aorta.
Patient subsequently underwent Endo-Vascular Aortic Repair (EVAR) and stayed one night in the hospital.
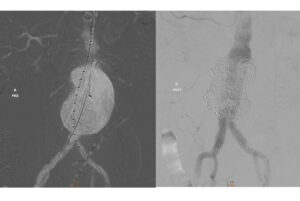
The infrarenal abdominal aortic aneurysm has been successfully treated with EVAR and patient remained well for 2 years.
Case Study 2
Patient presented with a persistent cough and increasing sac size in the mid-descending aorta following a previous thoracic Endo-Vascular Aortic Repair (TEVAR).
A catheter was inserted into the femoral artery and positioned above the old stent graft, where a new graft was deployed to reline the existing TEVAR.

There were no leaks post-closure with good flow.
Case Study 3
Patient presented with a thoracic aortic aneurysm(TAA) and a small infrarenal abdominal aortic aneurysm(AAA). The decision was made to perform a TEVAR with right subclavian chimney stenting and aneurysm sac coil embolization.
Stents were positioned in the affected blood vessels and deployed, allowing good flow to be restored to the left vertebral artery. Sac embolization was also done with coils which resulted in a good seal of the sac with no leaks.

The patient had stable blood pressure and good right radial pulse following the procedure. He was discharged on 1st post-op day. His aneurysm continued to shrink and he remains well 3 years later.
Aortic Dissection
Aortic dissection occurs when there is a tear in the aortic wall, resulting in blood flowing between the layers of the artery. It can lead to organ failure by disrupting blood flow to organs supplied by the aorta.
Severe chest pain and abdominal pain
- Uncontrolled hypertension
- Soft tissue diseases such as Marfan syndrome, Ehlers-Danlos syndrome, Loeyz-Dietz syndrome
- Aortic trauma
Diagnosis is done with a contrast CT scan to reveal the location of the tear in the aortic wall, and the extent of the dissection.
Our immediate priority will be to control elevated blood pressure so that the dissection does not worsen. Following this, surgical repair or minimally invasive EVAR may be performed to address the tear in the aortic wall.


